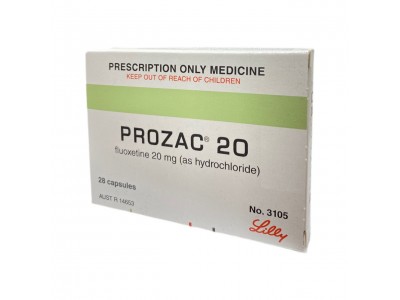
When taking Prozac (fluoxetine), it is important to be aware of potential interactions with other medications. Prozac is a selective serotonin reuptake inhibitor (SSRI), and certain drugs can interact with it, leading to serious side effects or reduced effectiveness.
One major concern is the combination with monoamine oxidase inhibitors (MAOIs), such as phenelzine or tranylcypromine. Taking Prozac with MAOIs can lead to serotonin syndrome, a potentially life-threatening condition characterized by high levels of serotonin in the brain. Therefore, there should be a gap of at least 14 days between stopping an MAOI and starting Prozac, and vice versa.
Other medications that can increase the risk of serotonin syndrome when taken with Prozac include other SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants, certain pain medications like tramadol and meperidine, and some over-the-counter supplements like St. John’s Wort.
Prozac can also interact with blood thinners such as warfarin, increasing the risk of bleeding. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin can also increase the risk of bleeding when taken with Prozac.
Certain antipsychotic medications, including pimozide and thioridazine, should not be taken with Prozac due to the risk of serious heart-related side effects, including QT prolongation, which can lead to potentially fatal heart rhythm abnormalities.
Additionally, Prozac can interact with medications that affect the enzyme CYP2D6, such as certain antiarrhythmics and some beta-blockers, potentially leading to increased levels of these drugs in the blood and heightened side effects.
Always consult with a healthcare provider before starting or stopping any medication while on Prozac, as they can provide guidance based on individual health needs and the specific medications involved.