Clopidogrel and ticlopidine, like aspirin, are antiplatelet medications used to prevent strokes, particularly in patients who have had a prior stroke or have other risk factors for cardiovascular events. They work by inhibiting platelet aggregation, which reduces the likelihood of clot formation. However, their effectiveness and safety profiles differ from aspirin.
Clopidogrel is widely used and has been shown to be effective in reducing the risk of stroke. In the CAPRIE (Clopidogrel versus Aspirin in Patients at Risk of Ischaemic Events) trial, clopidogrel demonstrated a slight but statistically significant advantage over aspirin in reducing the combined risk of ischemic stroke, myocardial infarction, and vascular death. It is often preferred for patients who cannot tolerate aspirin or have a contraindication to its use, such as a history of gastrointestinal bleeding or aspirin allergy.
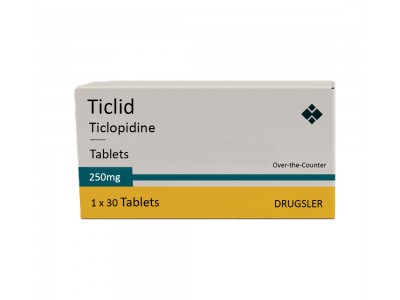
Ticlopidine was one of the earlier alternatives to aspirin and is effective in preventing stroke. However, its use has significantly declined due to its side effect profile, which includes a higher risk of hematologic complications such as neutropenia and thrombotic thrombocytopenic purpura (TTP). Clopidogrel is generally preferred over ticlopidine due to its more favorable safety profile and similar efficacy.
Aspirin has long been a mainstay in stroke prevention due to its proven efficacy, low cost, and wide availability. It reduces the risk of recurrent stroke by about 22% compared to placebo. Despite its benefits, it can cause gastrointestinal irritation and bleeding, which limits its use in some patients.
In summary, clopidogrel is considered at least as effective as aspirin in preventing stroke, with a better side effect profile compared to ticlopidine. Ticlopidine is effective but less commonly used due to its higher risk of serious side effects. The choice between these medications often depends on individual patient characteristics, tolerance, and the presence of contraindications to one or another of the drugs.